CPT 98981 Guide: Scaling RTM for High-Acuity Patients
Going the Extra Mile: Understanding CPT 98981
Remote Therapeutic Monitoring (RTM) is designed to bridge the gap between clinical visits. By leveraging digital platforms to collect non-physiological data such as therapy adherence, pain levels, and functional response, providers can monitor patient recovery in real-time.

While standard RTM codes cover routine management, CPT 98981 exists for the patients who require significant, “high-touch” intervention. It is the mechanism that allows RTM to scale from simple monitoring to intensive management for complex cases.
What is CPT 98981?
CPT 98981 is the “Add-On” code for Remote Therapeutic Monitoring Treatment Management.
Unlike the other RTM codes, CPT 98981 cannot be billed alone. It is designed to capture each additional 20 minutes of interactive communication and treatment management services provided in a calendar month, after the initial 20 minutes has been met.
The “Stacking” Logic:
- Tier 1: The first 20 minutes of care = CPT 98980.
- Tier 2: The next 20 minutes of care = CPT 98981.
Why CPT 98981 Matters for Modern Clinics
In a value-based care environment, the patients who need the most help are often the most expensive to manage. Before RTM, a therapist might spend 40 minutes on the phone with a struggling post-op patient and get paid $0 for that time.
CPT 98981 solves this problem. It ensures that when you dedicate extended time to managing complications, adjusting care plans, and guiding high-risk patients, your practice is reimbursed for that expertise. It turns “high-maintenance” cases into sustainable revenue.
The Math: When to Bill This Code
Billing CPT 98981 requires precise time tracking. You generally need to hit a 40-minute total threshold within one calendar month to trigger this code.
- 0–19 mins: No billing (under current 2025 rules).
- 20–39 mins: Bill CPT 98980 (1 Unit).
- 40+ mins: Bill CPT 98980 (1 Unit) + CPT 98981 (1 Unit).
Note: If a complex case requires an hour of management (60 mins), you would bill 1 unit of 98980 and 2 units of 98981.
Challenges in Implementation
Because CPT 98981 generates higher reimbursement, it comes with higher expectations for compliance.
- Documentation Rigor
You cannot simply check a box. CMSrequires proof that the additional time was medically necessary.
- The EMBODI Solution: Our platform logs every interaction. When you use EMBODI to review data or message patients, we create a timestamped audit trail that justifies exactly when and why you went “overtime” on a patient’s care.
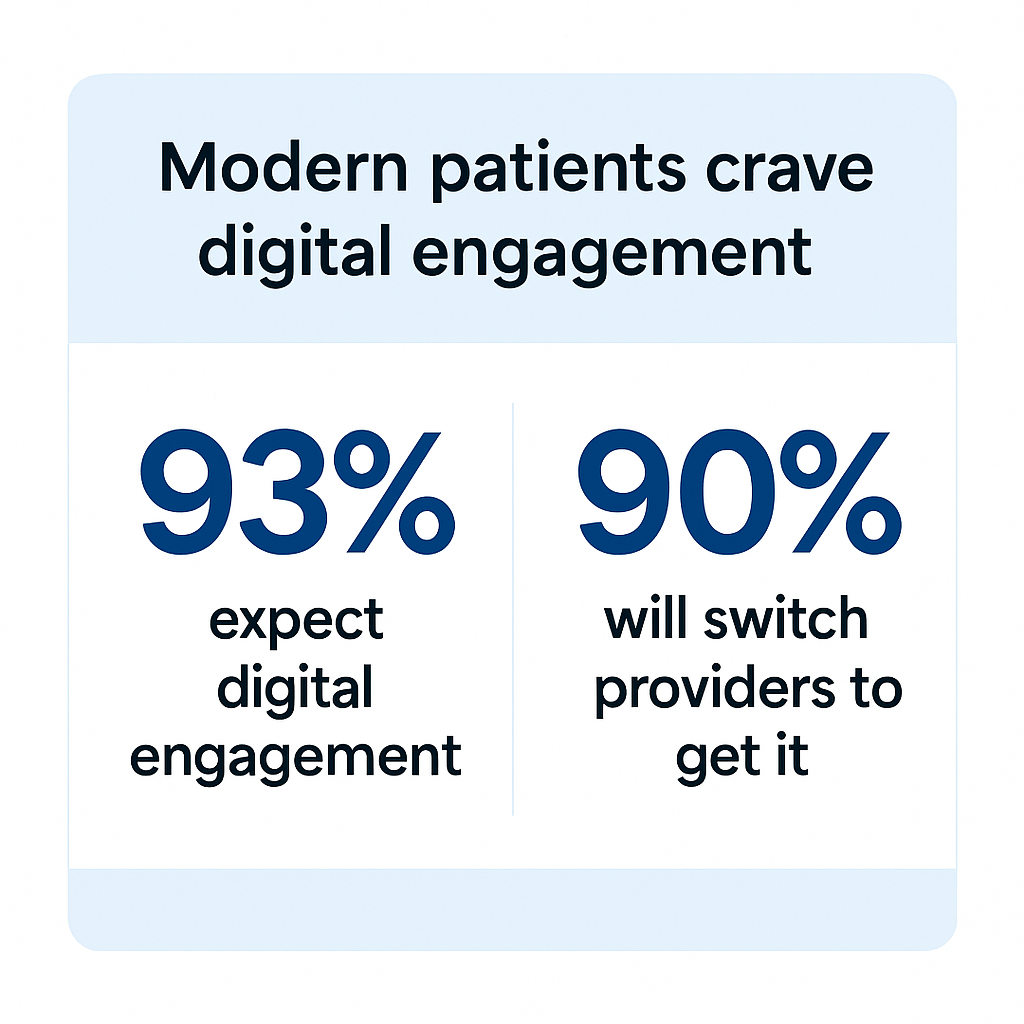
- The “Engagement” Drop-off
It is hard to manage a patient for 40 minutes if they stop logging data after Week 1.
- The EMBODI Solution: We use automated patient engagement tools—like gamification and smart notifications—to keep patients active in the app. Higher engagement leads to more data, which leads to more billable management time.
Best Practices for CPT 98981
To use this code effectively without triggering audits, follow these three rules:
- Reserve it for High-Acuity Cases
If you are billing CPT 98981 for every single patient, that is a red flag. Use this code for patients with:
- Post-surgical complications (e.g., stiffness, infection risk).
- Chronic pain requiring extensive behavioral coaching.
- Multi-trauma rehabilitation.
- Interactive Communication is Mandatory
You cannot bill this code solely by looking at a dashboard. At leastsome of this time must include interactive communication (phone, video, or secure messaging) with the patient or caregiver. - Document the “Pivot”
Your clinical notes should reflect action.Don’t just say “Reviewed data.” Say “Reviewed data indicating regression in flexion; spent 15 minutes via video call correcting form and 10 minutes adjusting HEP parameters.”
Stay Tuned: Preparing for 2026
While CPT 98981 is the standard for complex care today, the rules for time-based billing are evolving with the new year.
In January, we will release our full “2026 RTM Code Guide.”
We will provide a detailed breakdown of how 2026 regulations will impact documentation for these high-value add-on codes.
Disclaimer: The information contained in this document does not, and is not intended to, constitute legal, billing, or regulatory advice or guidance. All information, content, and material is for general information purposes and independent review and/or counsel should be obtained before making any legal or billing decisions.